Coeur d'Alene Ultrasound
Whole Breast Ultrasound Screening
Finally! Direct access to Early Cancer Detection…
Early Detection is the Key!
Keep reading to see why adding Whole Breast Ultrasound Screening to
your breast health regimen is smart prevention. Now you can be your own
best advocate in your breast health!
The Key to understanding the most effective means of early detection for you is knowing your breast tissue type. This is the critical information most women have not been able to obtain through their healthcare providers or mammograms…until recent changes in state laws began to require it!
An Inexcusable Fact: 70% of the women we lose each year to breast cancer have the type of tissue which often hides cancers on mammography, known as Dense Breast Tissue (DBT).
The Problem: In women with DBT, mammography and physical exams miss small, much more easily treatable cancers a staggering 50-60% of the time! Why? Because breast cancers and dense breast tissue both appear white on the mammogram image. For the radiologist who reads that mammogram, it’s much like trying to find a small snowball in a snowstorm. Since 40-50% of women have dense breast tissue, it’s not hard to see that half of the time mammograms and physical exams are just not enough!
The Solution: Whole Breast Ultrasound Screening, when performed by an ARDMS-registered sonographer (or a sonologist) with proper skills and experience specific to breast imaging, can increase the detection of cancer from approximately 48% to 97% in women with DBT. Hopefully your report will come back completely normal! But if we can find a small cancer early, treatment is much less invasive, chemo and radiation are usually unnecessary, and success stories skyrocket! Importantly, with ultrasound we can image all the breast tissue, including tissue closest to the chest wall and directly beneath your collar bone, as well as the axilla. Axillary breast tissue is the tissue that extends into the underarm area. Most women have never been informed that mammography is simply not capable of screening these areas of breast tissue for cancer. It’s surprising when you realize that substantial amounts of your breast tissue will actually never be screened if mammography is the only type of imaging you rely on! Why? When you have a mammogram, the breast is basically inserted between two plates and the plates squeeze the tissue. It’s not possible to position a woman in such a way that the breast tissue which extends into her underarm area can also be inserted between the plates. The same is true with the breast tissue which extends up beneath your collar bone. But don’t worry! We’ll be able to screen all your breast tissue when you come in for your Whole Breast Ultrasound Screening! Trina and Travis have each performed thousands of breast ultrasound exams over their 20 years as ARDMS-registered sonographers.
ADVANTAGES OF WHOLE BREAST ULTRASOUND…
● PAINLESS/NO COMPRESSION
● NO RADIATION
● NO HEAVY METAL CONTRAST AGENTS
● IMPLANT SAFE
● CONVENIENT
● AFFORDABLE
FAQs
+ What is Dense Breast Tissue (DBT)?
+ Mammography’s Limitations with DBT
+ How does Breast Ultrasound present a solution?
+ What are the potential advantages of Handheld Ultrasound Screening over some of the ‘Automated’ options?
+ What is Doppler Evaluation?
+ Why are Doppler and Elastography useful in evaluating for breast cancer?
+ Is ultrasound technology user dependent?
+ Who will be performing my screening breast ultrasound Exam?
+ Who will be the reading radiologist for my screening breast ultrasound?
+ Are Breast Ultrasound Screenings painful like a Mammogram?
+ Do you require Mammography before getting Whole Breast Ultrasound?
+ What should I expect the day of my Ultrasound appointment?
+ Do you accept Insurance?
+ What is the cost?
+ Do I need a physician’s referral to get this screening?
+ When will I receive my ultrasound results?
+ How do I make an appointment for a Whole Breast Ultrasound Screening?
+ Videos and References
What is Dense Breast Tissue (DBT)?
Dense breast tissue is composed of significantly more fibrous or glandular tissue than fattier breast tissue. Approximately half of women in the United States have dense breast tissue.

Breast Tissue Types: (a) almost entirely fatty, ( b) scattered fibroglandular tissue, (c) heterogeneously dense, and (d) extremely dense [4]
What is the Health Risk of having Dense Breast Tissue (DBT)?
70% of the women we lose each year to breast cancer are women with DBT. This is because early detection of small, and therefore much more easily-treatable, lesions simply does not happen 50-60% of the time using only mammography and physical exam.
How do I know if I have DBT?
If you have ever had a mammogram, you can inquire if you have DBT. A radiologist can determine the density of a woman’s breasts by examining a mammogram. If you have a report, make sure it is the report that is generated by the radiologist and not a ‘form’ letter. Read the report carefully and look for descriptions of your breast tissue type. ‘Heterogeneously dense’ and ‘extremely dense’ tissue, as classified by the appearance on mammography (see images above), are the two tissue types which are considered ‘dense breasts.’
On March 28,2019 the Department of Health and Human Services and the FDA announced changes to the MQSA (Mammography Quality Standards Act) to include reporting of dense breast tissue to the patient. Are You Dense Advocacy, Inc. has been working on the proposed rule changes for over ten years. There are now 23 States that have a law that requires disclosure of DBT on your mammography report.
Watch this short YouTube clip of Nancy Capello.
Nancy is the founder of Are You Dense Advocacy. A tremendous wealth of information can be found at www.AreYouDense.org.
Mammography’s Limitations with DBT
On a mammogram, dense tissue appears white and cancerous tumors also appear white making it nearly impossible for the reading radiologist to "see" the tumor. It's like trying to find a small snowball in a snowstorm.

A 43-year-old woman with extremely dense breast tissue. Dense tissue obscures a breast cancer that is easily visible with ultrasound imaging. (a,b) Craniocaudal (CC) and mediolateral oblique (MLO) digital mammography. (c) Handheld high-resolution ultrasound demonstrates a 1.2 cm irregular mass, denoted by calipers in the image, which was biopsied and proven to be invasive ductal carcinoma. [4]
According to the American Journal of Roentgenology “The sensitivity of mammography for the detection of breast cancer is 85%. However, in women with dense breast tissue, the sensitivity of mammography is reduced to 47.8–64.4%” [3] Since studies confirm that mammography alone misses cancer detection for approximately half the women in the United States, a much more trustworthy breast health regimen involves the addition of whole breast ultrasound or MRI to your annual mammogram.
How does Breast Ultrasound present a solution?
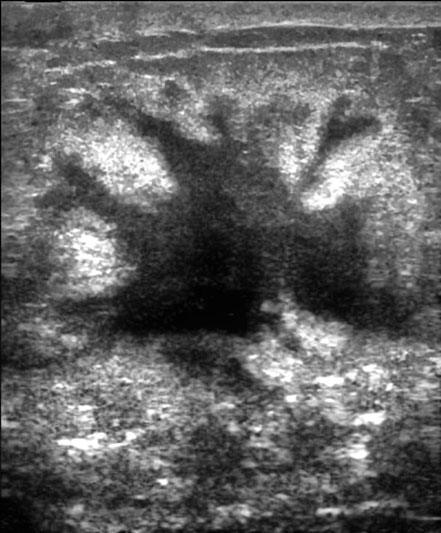
With proper ultrasound imaging technique, cancers often show up as a dark area surrounded by much brighter dense breast tissue. A skilled sonographer can maximize the quality of the images which will be sent to the radiologist by optimizing numerous settings on the ultrasound machine throughout the course of the exam.
 Breast ultrasound has been shown to increase early detection rates of
breast cancer from approximately 48% to 97% in women with dense breasts.
Whole Breast Ultrasound is not only able to detect smaller lesions earlier, it
is also able to detect cancer in three areas of your breast that cannot
be visualized using mammography alone
. Many people are not aware that mammography cannot reach breast tissue
closest to the chest wall, directly beneath the collar bone, or in the
axilla. The axilla is the area of breast tissue that extends partially into
the armpit. The axilla contains lymph nodes which can be enlarged during
times of heightened immune response, such as when the body may be fighting
a viral or bacterial infection or a cancer. Our whole breast ultrasound
screenings include evaluation of these three areas where breast cancer
could easily go undetected by mammography.
Breast ultrasound has been shown to increase early detection rates of
breast cancer from approximately 48% to 97% in women with dense breasts.
Whole Breast Ultrasound is not only able to detect smaller lesions earlier, it
is also able to detect cancer in three areas of your breast that cannot
be visualized using mammography alone
. Many people are not aware that mammography cannot reach breast tissue
closest to the chest wall, directly beneath the collar bone, or in the
axilla. The axilla is the area of breast tissue that extends partially into
the armpit. The axilla contains lymph nodes which can be enlarged during
times of heightened immune response, such as when the body may be fighting
a viral or bacterial infection or a cancer. Our whole breast ultrasound
screenings include evaluation of these three areas where breast cancer
could easily go undetected by mammography.
What are the potential advantages of Handheld Ultrasound Screening over some of the ‘Automated’ options?
Adding one of the various Automated Breast Ultrasound Screenings to your annual breast health regimen is certainly much better than not adding any ultrasound imaging, particularly if you have DBT. However, in experienced hands, Handheld Ultrasound can detect up to twice as many small cancers as any Automated Ultrasound. Why? All breasts have areas where the tissue is less dense and areas where the tissue is more dense, regardless of which tissue density category a mammogram report says they are in. A suspicious lesion within an area of less dense tissue is best represented with machine settings which are different than those which are ideal for a lesion surrounded by tissue which is more dense. Due to these constantly varying densities from region to region, breast tissue will always be best imaged by an experienced, ARDMS-registered sonographer (or a sonologist) using Handheld Ultrasound. A ‘set it and forget it’ approach to acquiring images and/or video clips of breast tissue will never be considered the gold standard or superior to Handheld Ultrasound. Why? Because real-time evaluation with a handheld transducer allows for minute-by-minute image optimization of any suspicious tissue or lesion in order to best characterize if it is cystic or solid, has smooth or irregular borders, is vascular or non-vascular, is hard or soft, etc. These critical, real-time technical adjustments required to produce images of the highest possible quality simply do not occur during any Automated Breast Ultrasound. A skilled sonographer has to consider the pressure that is being applied to the breast, the angle of the transducer, and the proper utilization of the ultrasound machine’s capabilities, including Gain, Focus, TGC, Doppler and Elastography settings, etc. Whether or not these minute-by-minute adjustments occur, and result in fully-optimized images for the radiologist, is ultimately crucial to the sensitivity and overall accuracy of your report. The more we can fully characterize any suspicious tissue for our radiologist, the lower the likelihood a False Positive or False Negative report will be generated. This is important because a False Positive report can result in a costly, uncomfortable and unnecessary biopsy on breast tissue that is not cancerous.
What is Doppler Evaluation?
Doppler is a feature that allows us to evaluate for blood flow within a lesion.

A: Grayscale image of palbable breast mass that could be cystic or solid
B: color Doppler images demonstrate internal vessels, thus is a solid lesion.
What is Elastography?
Elastography is a feature on an Ultrasound imaging machine that allows the sonographer to demonstrate the density or hardness of a lesion to the reading radiologist.
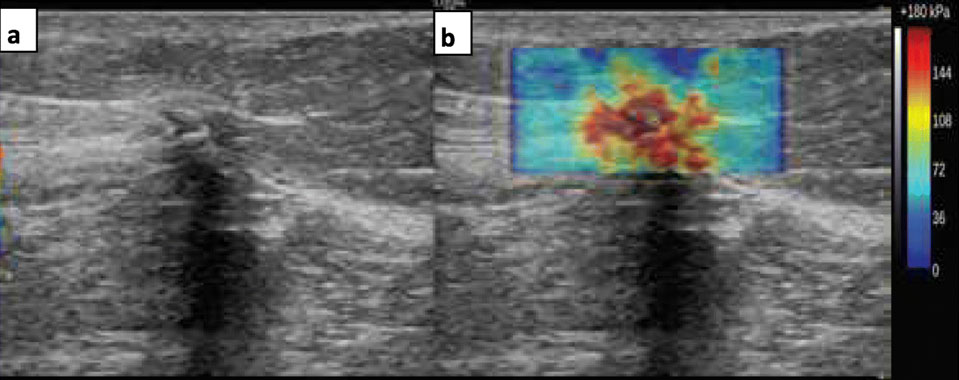
Why are Doppler and Elastography useful in evaluating for breast cancer?
Doppler and Elastography are powerful sonographic tools which can aid in differentiating between cancerous and non-cancerous lesions. Vascular flow (blood flow) within a lesion can be an indicator that the lesion may more-likely be malignant. Cancerous masses are typically more dense or hard than those without malignancy. If a lesion is questionable for cancer but is shown with Elastography to be the same density as the surrounding breast tissue, the concern level for cancer may decrease. The correct utilization of Doppler and Elastography provides more information to our radiologist and results in a lower rate of false positives, thereby reducing unnecessary biopsies. For example, if a suspicious small, lesion shows minimal or no internal blood flow and is soft, your care provider may encourage you to have a follow-up (rather than biopsy), since the risk of malignancy is lower. On the other hand, if the questionable lesion is vascular and hard, your doctor may want to biopsy or maybe even go straight to removal of the lesion. Elastography has become a game changer. It can provide a tremendous amount of information on potentially suspicious lesions to the reading radiologist. Wherever you decide to go for your breast ultrasound screening, be sure they evaluate any suspicious tissue with both doppler and elastography.
Is ultrasound technology user dependent?
Unlike CT and MRI, ultrasound technology is incredibly user dependent. The quality of the images obtained, and ultimately the sensitivity and accuracy of your results, often depends greatly on the caliber of training and level of expertise the performing sonographer brings to the exam table. Why? Isn’t there some fairly strong international uniformity between the quality of one ultrasound image and another? No, unfortunately. Have you ever heard of someone being told they were having a girl after an ultrasound exam and they ended up having a boy? A cancerous breast lesion is usually much smaller anatomically than the parts you need to evaluate during a baby’s gender determination! Breast ultrasound screenings should be performed by an ARDMS-registered sonographer (or a sonologist) with training and experience specific to breast ultrasound imaging.
Who will be performing my screening breast ultrasound Exam?
All exams are performed by ARDMS-registered, highly-experienced breast imaging specialists. Trina and Travis Armstrong have each performed thousands of breast ultrasound exams in their respective 20 years of experience as diagnostic medical sonographers. Not rookies, they are both very thankful for the years they were able to spend optimizing their skills at a primary Harvard teaching hospital in Boston, Beth Israel Deaconess MC.
Who will be the reading radiologist for my screening breast ultrasound?
All of our breast ultrasound screenings are read by our board-certified radiologist.
Are Breast Ultrasound Screenings painful like a Mammogram?
There is no comparison! During your breast ultrasound, we apply warm gel and use a handheld transducer to take images of your breast tissue. There’s no compression, no radiation and no pain!
Is Breast Ultrasound a replacement for Mammography?
No. Coeur d’Alene Ultrasound advocates that women add whole breast ultrasound screenings to their current regimen. Mammography can pick up microcalcifications that are not easily detected with ultrasound. However, ultrasound can often see small lesions that mammography can miss, especially in women with DBT. Mammography is efficient in detecting cancer in women with fattier breast tissue. Ultrasound can characterize lesions more effectively in fatty or dense breast tissue. Mammography and Ultrasound often deliver higher specificity and sensitivity (overall accuracy) when used together. However, it has become much more evident, particularly in women with dense breast tissue (DBT), that mammograms and physical exams are simply not sufficient. 40-50% of women have DBT and 70% of the women we lose each year to breast cancer have this type of tissue, which frequently hides cancers on mammography.
Do you require Mammography before getting Whole Breast Ultrasound?
No. It is you and your care provider’s decision to get a mammogram before or after your whole breast ultrasound screening. Currently, mammography is recommended for routine breast cancer screening by the ACS. If you have had one or more recent mammograms, please bring your reports with you, as well as all of your images in DICOM format on a small and portable USB drive (aka thumb drive). We strongly recommend you delay scheduling your appointment with us until you’re in possession of all your relevant mammogram reports and images in DICOM format. We will upload them to our secure server so our radiologist can compare them to your new ultrasound images.
What should I expect the day of my Ultrasound appointment?
Once you arrive at our comfortable office, you will be asked to fill out a brief medical history. Once completed, we will provide you with a cloth drape to cover your chest area with before beginning the exam. An ultrasound probe with warm gel will be used to begin screening both breasts and axillary regions (medial underarm areas). No preparation is necessary.
Do you accept Insurance?
At this time, Coeur d’Alene Ultrasound does not accept Medicare, for screening breast ultrasound services. Many of the women who use our services will provide their payment receipt to their insurance companies so that the cost might be applied toward their out-of-network deductible. Other patients may be able to submit the receipt to their health share ministry and receive compensation. Each patient should consult with their individual health share ministry or insurance company to better understand their unique situation. Most FSA and HSA cards can be accepted, as long as there is a major credit card label on it.
What is the cost?
Our breast screenings include imaging of all your breast tissue, as well as targeted evaluation of any suspicious lesions with color doppler and elastography. Our radiologist’s reading fee is also included. Their report will be faxed to your health care practitioner, with another copy mailed directly to you. We love talking with our patients, but possible questions from your screening results should be discussed with your wisely-chosen healthcare practitioner. This is because we are sonographers, not practitioners, and it's not legal to practice medicine without a license. There is no tax and the total service fee is $375. We accept all major credit/debit cards and cash. Payment is due at the time of service.
Do I need a physician’s referral to get this screening?
Since this procedure is done on a fee-for-service basis, no prescription or referral from a doctor is required to obtain our whole breast ultrasound screening. We do need you to list your care provider’s name, phone number and fax number on your registration form. As we are sonographers, not physicians, you and your care provider must be the ones discussing your results and any applicable plans of care. If your care provider would like to send a referral, our fax number is 208.930.4154.
When will I receive my ultrasound results?
Your images will be read by our board-certified radiologist and their report will usually be faxed to your care provider within 24 hours after the completion of your whole breast ultrasound screening. A copy of this report will also be mailed to the address you provided on your medical form and delivered via US mail within 7-10 business days (excluding weekends and holidays) following the date of your appointment.
How do I make an appointment for a Whole Breast Ultrasound Screening?
Just give us a ring! If we happen to miss you, just leave us a message and we’ll get right back to you! 208.261.2520. If you contact us by email or text, response time may be just a little more delayed.
Videos:
Journalist Joan Lunden Discusses Her Breast Cancer Diagnosis and Treatment
The Cancer Risk You Haven’t Heard of...
If You’re Dense, You Need to be Smart | Chiqeeta Jameson | TEDx
Nancy Capello founder of Are You Dense:
Studies, References and Resources
1. Breast Density Implications and Supplemental Screening (Women with DBT should add whole breast ultrasound to their regimen. There's a shortage of experts in Handheld Breast Ultrasound. Automated breast ultrasound is improving, but the higher number of false positive results needs to be improved.)
(click here to read more)
2. A Handy Guide to Dense Breasts (Handheld Ultrasound in skilled hands is more sensitive than automated)
(click here to read more)
3. Wherever you plan to go for your ultrasound screening, verify they will include Elastography! Read about how elastography is a game changer for distinguishing benign solid lesions from malignant solid lesions. Fewer false-positive results! Minimize recommendations for a biopsy!
(click here to read more)
4. Screening Breast Ultrasound: Past, Present and Future (Women with DBT should add whole breast ultrasound to their regimen. There's a shortage of experts in Handheld Breast Ultrasound. Automated methods are showing some promising workflow benefits, but often-times any findings will require another appointment for a targeted Handheld Ultrasound with superior resolution and elastography.)
(click here to read more)
5. Are you dense brochure
(click here to read more)
6. Are you dense website
(click here to read more)

